A traumatic event causing injury to an intervertebral disc may also cause subtle injuries to the bones around the disc. During an extreme lateral flexion injury (shown in the image below), the edges of the bone are driven together, injuring both the disc and the bone. As the bone/disc junction heals, overgrowths referred to as osteophytes may form.
Osteophytes take weeks or months to develop following a traumatic event; therefore, any osteophytes that are present soon after a traumatic event are likely pre-existing.
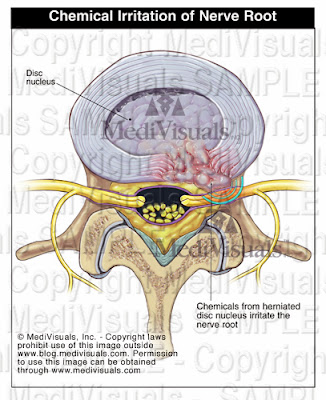
The osteophytes themselves may compress the neural elements as in the illustration above; however, in most situations, the osteophytes are a part of an OSTEOPHYTE/DISC COMPLEX. This is when the osteophytes and disc extend beyond their normal limits and compress the neural elements (spinal cord, nerve roots). In cases where osteophytes may have pre-existed a traumatic event, worsening of the disc bulge could occur following the trauma, resulting in new or aggravated symptoms.
Sometimes disc and ligament injuries occur on the same side as the force of impact. Other times, they occur on the opposite side. Injuries to the disc on the same side as the force are the result of stretching and tearing forces. On the opposite side, compression forces result in tears and micro fractures of the tissues and bones. (see illustration below). Osteophytes and facet hypertrophy can also form following injuries to intervertebral discs and ligaments. Injuries to the discs and ligaments result in instability and excessive motion of the joints that, in turn, results in constant trauma to the bone/disc and ligament junctions. This ongoing trauma results in overgrowth of the bones as it continually cycles through episodes of healing and reinjury.